Landscape of Opportunity: 5th Edition
Introduction
California’s Black, Indigenous, and other People of Color (BIPOC)* continue to experience persistent health disparities arising from systemic racism that blocks access to the resources and opportunities needed to achieve good health. In turn, these disparities are not just differences, but inequities, which include a safety net that fails to provide every human-being with their basic needs for health care, nutrition, and housing.
Although federal and state legislation including the Affordable Care Act (ACA, 2010) and Medi-Cal expansions have greatly improved the safety net’s reach, these changes are insufficient. Lack of interpreter services, culturally competent care, geographically distant providers and high cost-sharing remain barriers to essential health care for communities of color.
These health disparities take place in the context of a diverse California. Already, over half of all Californians identify as non-White, highlighting the importance of eliminating these long-standing inequities. The COVID-19 pandemic increased the urgency of this task, demonstrating how heath disparities and unequal access to health care, jobs and housing disproportionately harm communities of color, but in the end hurt us all.
The Landscape of Opportunity provides an overview of the current state of health disparities and challenges facing California. It serves as a resource for advocates and policymakers alike, highlighting key areas where inequities persist that are ripe for future action to advance health equity.
*We begin with BIPOC to highlight the individualities of people of color, while also acknowledging preferences and language vary and evolve. Throughout the remainder of this document, we use the term “communities of color” to emphasize the value of community and in contrast to the White population. In addition, many terms are used interchangeably (e.g., Hispanic/Latino/Latinx, Black/African American), which largely reflects variety in data collection.
Section One: California’s Diverse Communities
As the nation’s most populous state, California’s diversity contextualizes the urgent needs and opportunities to advance health equity. California communities are comprised of people of all races and ethnicities who speak many languages, making California one of the most diverse states in the nation. As the State seeks to close the health disparities gap, success lies with addressing the varied and specific needs of communities of color, ensuring that no one is left behind.
Over Half of California’s Population Belongs to a Community of Color
Source: U.S. Census Bureau American Community Survey
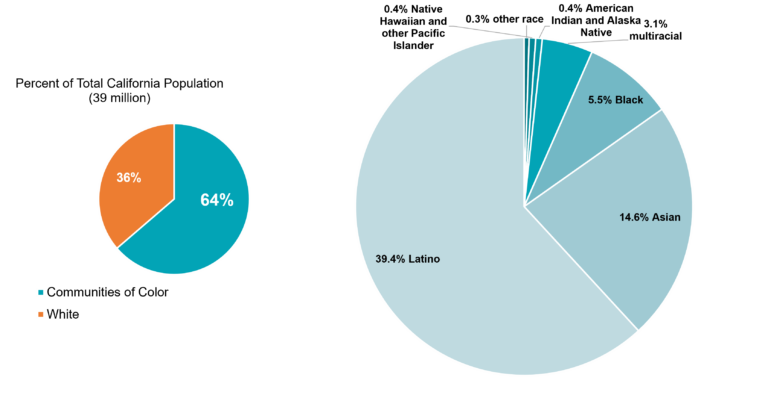
Communities of color comprise 64% of the state’s 39 million people.
The percentage is much higher in several of California’s 58 counties including Imperial (91%), Merced (75%), Los Angeles (75%), and San Bernardino (75%).
For more information, including statistics for other states and the country
Californians Speak Many Languages

Source: U.S. Census Bureau American Community Survey
44% of Californians (age 5 years and older) speak a language other than English at home. Of these persons, 17% indicated they speak English less than “very well.”
Many California households speak both English and Spanish at home. In Imperial county nearly 47% of individuals surveyed speak English and Spanish at home, followed by 39% in Tulare and 34% in San Benito. In Los Angeles county, home to almost 10 million Californians, 29% of individuals speak both English and Spanish at home.
Source: https://healthpolicy.ucla.edu/chis/data/Pages/GetCHISData.aspx
California is Home to Many Immigrant Families
California has a vibrant immigrant community that spans generations.
More than 1 in 4 Californians (27%) are immigrants, with nearly half (46%) of all California children having at least one parent who was born in a country other than the U.S.
Sources: U.S. Census Bureau American Community Survey
Section Two: Disparities in Health Status
Communities of color face persistent health disparities including higher rates of asthma, diabetes, certain mental health conditions, and poor oral health resulting in a shorter life span, less wealth, and less opportunity.
These disparities cannot be attributed to any inherent personal characteristics, but they are the product of systemic racism – policies and institutions that hurt communities of color by blocking their access to resources and opportunities through unjust practices such as residential segregation, biased lending practices and job discrimination. The COVID-19 pandemic hit communities of color hard, highlighting the dire need to reduce disparities and increase preparedness.
COVID-19 Widened Health Disparities
As a new leading cause of death, COVID-19 reduced U.S. life expectancy overall, but in 2019 Black, and American Indian and Alaska Native populations were the only communities with life expectancies under 75 years (74.8 y and 71.8 y, respectively).
While Californians enjoy a longer life expectancy than the nation as a whole, racial and ethnic disparities persist with Blacks having the lowest life expectancy at 75.1 years. Nationally and locally, deaths from COVID-19 did not occur evenly.
By April 2023, cumulative statewide data show Native Hawaiian and Pacific Islander communities suffered a COVID-19 case rate 3x that of their White counterparts and a death rate 1.7x greater. Black and Latinx communities also experienced higher death rates. In total, over 64,000 BIPOC lives have been lost to COVID-19.
Sources: https://www.cdc.gov/nchs/data/vsrr/vsrr023.pdf
https://www.chcf.org/wp-content/uploads/2021/10/DisparitiesAlmanacRaceEthnicity2021.pdf.
Communities of Color and COVID-19: Cumulative Deaths and Cases
(Persons 50-64 years)

Note: 121 deaths had no race/ethnicity information.
Source: https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/Age-Race-Ethnicity.aspx#, April 7, 2023
Retirement is one of life’s milestones, but COVID-19 resulted in numerous premature deaths in California.
As the top 4 sets of bars shows, the Hispanic, Black, Native Hawaiian and other Pacific Islander, and American Indian and Alaska Native communities were not only hit hard by COVID-19 cases (teal bar), but deaths (orange bar) among persons 50-64 years.
Given their proportion of the California population (yellow bar), these communities unequally bore the burden of COVID-19.
Learn More: https://calmatters.org/california-divide/2022/07/california-life-expectancy/.
Communities of Color Have Higher Rates of Chronic Conditions
Beyond advancing age, many chronic conditions such as asthma, diabetes and certain mental health conditions are risk factors for severe illness from COVID-19. Communities of color were already experiencing high rates of chronic illness prior to the COVID-19 pandemic, placing them at greater risk for poor health outcomes.
Source: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
Asthma Disparities

*Unstable estimates due to small numbers
Source: https://healthpolicy.ucla.edu/chis/data/Pages/GetCHISData.aspx
Within California, Black, multiracial and American Indian and Alaska Native communities experience high rates of asthma (21%, 21% and 20%, respectively). Overall, 15% of all Californians have been diagnosed with asthma, underscoring how poor air quality and living conditions impact us all.
Learn more about asthma in California:https://www.cdph.ca.gov/Programs/CCDPHP/DEODC/EHIB/CPE/Pages/CaliforniaBreathingData.aspx
Diabetes Disparities

*Unstable estimate due to small numbers
Source: https://healthpolicy.ucla.edu/chis/data/Pages/GetCHISData.aspx
Communities of color have higher rates of diabetes in California compared to their White counterparts (9%), especially Native Hawaiian and Pacific Islander (29%), American Indian and Alaska Native (22%), Black (15%) and Latino (13%) communities. The likelihood of developing and managing diabetes depends on access to affordable tasty and healthy food as well as opportunities for physical activity. Diabetes and pre-diabetes (elevated blood sugar not high enough to be considered diabetes) are worsened by cheap, fast calorie-dense food options and a lack of convenient safe spaces for physical activity – both of which are more common in lower-income diverse neighborhoods.
Disparities in Diagnosis
The percentage of Asians diagnosed with diabetes (10%) is relatively low, but diabetes is severely under-diagnosed in this population. Because diabetes is a progressive condition, it is estimated 1 in 5 people nationally don’t know they have it, but this increases to 1 in 3 for Asian Americans. Moreover, in California, it has been estimated almost half of all adults have pre-diabetes, including over 1 in 3 young adults (18-39 years) of color.
Sources: https://www.cdc.gov/diabetes/library/spotlights/diabetes-asian-americans.html https://healthpolicy.ucla.edu/publications/search/pages/detail.aspx?PubID=1472
Mental Health Disparities

Adults with a Serious Mental Illness, 2019
Source: https://www.chcf.org/wp-content/uploads/2022/07/MentalHealthAlmanac2022.pdf
The COVID-19 pandemic not only took a severe toll on physical health, but also the nation’s mental health. Mental illness is common with almost 1 in 7 adult Californians having experienced a mental illness. Among those who are incarcerated the rate of mental illness is much higher (nearly 1 in 3 female, and 1 in 5 male inmates, respectively) than the overall rate.
Serious mental illness is relatively rare at 3.9% of Californians, it is highest for American Indian and Alaska Native communities (6.8%) and Black Americans (5.3%). Very low rates among Asian groups likely reflect under-diagnosis and treatment.
The rate of serious mental illness more than doubles (8.5%) among adults in families living in poverty (incomes <100% of the federal poverty level).
Poverty and incarceration are more common among communities of color due to systemic racism.
Learn More: https://cpehn.org/what-we-do-2/our-projects-2/building-towards-antiracist-governments/.
Sources: https://www.samhsa.gov/data/release/2021-national-survey-drug-use-and-health-nsduh-releases https://www.chcf.org/publication/2022-edition-mental-health-california/#related-links-and-downloads
Oral Health Disparities

Source: https://healthpolicy.ucla.edu/chis/data/Pages/GetCHISData.aspx
A healthy smile is more than cosmetic. Teeth impact our ability to communicate and eat, while untreated cavities can result in infection and tooth loss.
Poor oral health is common among communities of color with 36% of adult Latinos indicating the condition of their teeth is “fair or worse” (including no natural teeth) compared to 21% of White adults.
Section Three: Inequity in Health Care Delivery
A health care system not grounded in racial equity will result in racial inequity. The poor health status of communities of color is partly due to a health care system unable to meet their needs.
Presently, communities of color represent a disproportionate share of persons without any health insurance or Medi-Cal coverage (California’s health insurance program for lower-income persons). Moreover, while mental health and dental care are Medi-Cal covered benefits for adults, logistics like transportation and time-off work in addition to cost-sharing and a shortage of culturally competent providers remain barriers to care.
Covering approximately 13 million Californians (1 in 3), California’s Medi-Cal program is the largest Medicaid program in the country.
Sources: https://www.chcf.org/publication/2021-edition-medi-cal-facts-figures/https://www.dhcs.ca.gov/dataandstats/statistics/Pages/Fast_Facts.aspx
Inequities in Health Insurance Coverage

*unstable estimate due to small numbers
Source: https://healthpolicy.ucla.edu/chis/data/Pages/GetCHISData.aspx
Due to the Affordable Care Act (2010) and California’s Medi-Cal expansion, there have been significant gains in health care coverage among communities of color, but inequities remain. Communities of color generally have higher rates of uninsurance when compared to their White counterparts.
Learn More: About the Affordable Care Act
Nearly 1 out of 8 Latinos still lacks any health insurance. California’s further expansion of Medi-Cal to include low-income adults (ages 26-49 years) regardless of immigration status is due to go into effect January 2024. This change will reduce the uninsurance rate, especially among Latinos, but not eliminate it.
Source: https://laborcenter.berkeley.edu/californias-uninsured-in-2024/
Communities of Color are the Majority of Medi-Cal Enrollees

Percentage of Medi-Cal Enrollees (Communities of Color) 79.4%
Source: https://www.dhcs.ca.gov/dataandstats/statistics/Pages/Fast_Facts.aspx
While communities of color are 64% of California’s total population, they are nearly 80% of the Medi-Cal population, and this is driven by Black and Latino populations being over-enrolled by 50%.
Specifically,
- Black Americans are 5.5% of the California population, but 8.4% of the Medi-Cal population.
- Hispanic persons are 39% of the California population, but 59% of the Medi-Cal population.
Sources: https://www.dhcs.ca.gov/dataandstats/statistics/Pages/Fast_Facts.aspxU.S. Census Bureau American Community Survey
Covered California: Enrollment by Subsidy and Race/Ethnicity

Source: https://hbex.coveredca.com/data-research/
Covered California, California’s health insurance exchange under the Affordable Care Act provides coverage to more than 1.7 million Californians.
Sources: https://www.coveredca.com/; https://www.coveredca.com/newsroom/news-releases/2023/03/09 /
Communities of color, especially Latinos and Asian Americans more commonly have their premium subsidized compared to White enrollees reflecting their lower income status. While subsidies enable more Californians to have health insurance, further cost-sharing remains a barrier.
Learn More: https://cpehn.org/publications/ https://cpehn.org/what-we-do-2/policy-tracker/
Unaffordable Care Even with Insurance
The high cost of health care even with health insurance is not unique to California.
- A recent Gallup poll found 38% of Americans or a family member delayed medical care due to cost in 2022, up from 26% in 2021.
- Nationally, women, younger adults and lower-income persons were most likely to report postponing care.
- Analysis by race and ethnicity found Latino adults were more likely than other groups to find cost a barrier to care.
Sources: https://news.gallup.com/poll/468053/record-high-put-off-medical-care-due-cost-2022.aspx
https://www.healthsystemtracker.org/chart-collection/cost-affect-access-care/
High Mental Health Utilization by Age and Insurance
In 2020, about 1 out of 4 diagnoses in California emergency departments (ED) and inpatient settings were mental health disorders, substance use disorders, or both.
ED visits were more common among adults ages 19 to 39 years (40% of all ages), while inpatient hospitalizations were more common for persons over age 60 (40% of all ages). The expected payer was public insurance (Medi-Cal or Medicare*) for more than 2 out of 3 encounters.
*Medicare covers those age 65+ and persons with certain disabilities or end-stage renal disease regardless of age (https://www.medicare.gov/what-medicare-covers/your-medicare-coverage-choices/whats-medicare).
Unmet Mental Health Needs
Prior work indicates unmet mental health needs for communities of color enrolled in Medi-Cal (https://www.chcf.org/publication/mental-health-disparities-race-ethnicity-adults-medi-cal/). Recent 2022 data continue to show disparities among adults (21+ years) accessing mental health services:

Learn More: https://cpehn.org/what-we-do-2/our-networks/california-reducing-disparities-project/
https://www.chcf.org/publication/2021-edition-health-disparities-race-ethnicity-california/
Nationally: https://www.samhsa.gov/data/release/2021-national-survey-drug-use-and-health-nsduh-releases
Dental Care Barriers Persist
Senate Bill 97 restored adult dental benefits in the Medi-Cal program in 2018, but racial disparities in access persist, and access rates remain low overall.
Learn more: https://cpehn.org/publications/addressing-the-root-dismantling-systemic-barriers-to-oral-health-equity
While 24% of the non-Medi-Cal population indicates the condition of their teeth is “fair or worse” (including no natural teeth), this response jumps to 45% for the Medi-Cal population.
In addition, 29% of adult Californians have no dental insurance and are financially responsible for the full cost of prevention and treatments if they’re able to locate a provider. Lack of dental insurance is most common among the Latino population at 36%.
Source: https://healthpolicy.ucla.edu/chis/Pages/default.aspx?
Preventable Hospitalizations

A hospitalization is considered preventable when timely primary care could have maintained a person’s health and kept them out of the hospital. It also reflects the social determinants of health (SDoH), because transportation, housing, ease of communication, and payment for medications including delivery are influenced by social factors that impact health.
Black Americans (13.8%) specifically, followed by American Indian and Alaska Native communities (10.2%) in California, have rates of preventable hospitalizations substantially higher than other groups.
Discrimination in Health Care Delivery
The Listening to Black Californians project (2021 – 2022) sponsored by the California Health Care Foundation (CHCF) found:
- Almost 1/3rd of Black patients were treated unfairly by a healthcare provider
- Despite over 3/4ths of Black Californians putting forth considerable effort to receive appropriate preventive care and focus on their mental health
- Over 1/3rd of Black Californians have adjusted their speech and/or behavior to help the healthcare provider feel at ease.
- Black women, those who identify as LGBTQIA+, have a physical disability or mental health diagnosis are even more likely to report enduring racism and insufficient pain treatment.
Source: https://www.chcf.org/publication/in-their-own-words-black-californians-racism-health-care/
Learn More: https://www.healthaffairs.org/do/10.1377/forefront.20200108.34515/
Discrimination in Health Care Delivery Nationally, Among Older Adults
(60+ years)
When asked whether they had ever been treated unfairly and/or had their concerns dismissed while receiving health care because of their race/ethnicity, about 1 out of 4 Latinx and Black US older adults reported “yes.” In contrast, few White older patients felt the same.

Source: https://www.commonwealthfund.org/publications/issue-briefs/2022/apr/how-discrimination-in-health-care-affects-older-americans
Preferred Language in Health Care Delivery
A language other than English was desired in nearly 13% of all patient encounters statewide (2 million visits in 2020). The vast majority of patients preferred Spanish, but almost 300,000 patients wanted to speak in an Asian/Pacific Islander or Middle Eastern language.
Source: https://hcai.ca.gov/visualizations/preferred-languages-spoken-in-california-facilities/.
Community Health Workers
As of July 1, 2022, Medi-Cal began covering community health worker services. As trusted members of the community with lived experience, community health workers and promotores (CHW/P) can help fill the gap in culturally competent care. The COVID-19 pandemic highlighted the need for and value of CHW/P. CPEHN’s own People Power for Public Health survey (https://cpehn.org/assets/uploads/2022/08/CPEHN.PeoplePowerForPublicHealthReport-FINAL.pdf) found:
- More than two in five (44%) survey respondents noted that community-connected providers were most helpful when they or a loved one experienced a mental health crisis.
- Instead of having police respond to behavioral health crises, participants expressed a desire to engage with first responders who have expertise in behavioral health, including social workers, peer support specialists, and community health workers.
Sources: https://www.dhcs.ca.gov/community-health-workers
https://www.chcf.org/wp-content/uploads/2023/04/CHWPFactSheet52223.pdf
Learn More: https://www.cpehn.org/what-we-do-2/our-networks/community-health-workers-promotores/
Nationally: https://www.pcori.org/topics/community-health-workers
An Engaged Community is a Healthy Community

Source: https://healthpolicy.ucla.edu/chis/data/Pages/GetCHISData.aspx
Increasingly, studies indicate that community engagement – including voting, is tied to better health. At an aggregate level, states with lower voter participation have poorer health. Voting accessibility enables all members of society to participate in democracy. In 2022, the American Medical Association (AMA) declared voting a Social Determinant of Health (SDoH), recognizing that voting is fundamental to the enactment of social policies that influence health.
Nearly 1 in 3 California citizens is “sometimes to never engaged” in voting in national, state or local elections with stark disparities by race/ethnicity. Asian and Latino communities responded they are sometimes or never engaged in voting at about twice the rate of their White counterparts (43% and 40%, respectively, vs. 21%).
Sources: Blakeley, T., Kennedy, B., Kawachi, I. (2001). “Socioeconomic inequality in voting participation and self-rated health.” American Journal of Public Health. (1): 99–104. doi:10.2105/ajph.91.1.99. https://voiceproject.ucsf.edu/voting-and-health and https://catalyst.nejm.org/doi/full/10.1056/CAT.22.0368
Conclusion
Like the title of our publication, there is an opportunity for community members and policymakers to collaborate and reduce health disparities in California. The COVID-19 pandemic widened and exposed these disparities and the inequity behind them. Beyond the pandemic, anti-racist protests in the summer of 2020 launched discussions of historical racial discrimination, harm, and violence in many social sectors, including health care. Combined, we see the damage systemic racism has on the health and security of communities of color then and now.
Let’s use this opportunity to rebuild our public health and health care system’s foundation with the interests of communities of color in mind. For too long, their health and well-being have been afterthoughts in policymaking.
Equity in Health Care System Reform
The California Health Care Foundation funded the California Pan-Ethnic Health Network (CPEHN) to develop policy recommendations linking health care payment and delivery reform to health equity. Our recommendations for achieving equitable care and health outcomes are interlocked facets missing in our current system (https://cpehn.org/reports/centering-equity-in-health-care-delivery-and-payment-reform-a-guide-for-california-policymakers/). We must center equity in quality and payment, engage patients’ families and caregivers, and strengthen culturally and linguistically appropriate care. Integrating physical, behavioral, and oral health care, while holding health plans and systems accountable, will improve the health care system for everyone.
Equity in Public Health
Moreover, the COVID-19 pandemic underscored the need for improving the social determinants of health through a stronger equitable public health system. CPEHN’s People Power for Public Health (https://cpehn.org/publications/people-power-for-public-health/) aims to reform budget processes and reallocate resources (https://cpehn.org/arpascorecards) to address longstanding health inequities and chronic under-investment in an equitable public health infrastructure.
Equity in Data Collection
To support this effort, comprehensive disaggregated data is required. Too often, broad categories (e.g., Asian, Latino), missing data (e.g., sexual orientation gender identity, disability) or confusing catchalls (e.g., some other race) hamper policymakers and health care providers from equitable spending and tailoring care to maximize health outcomes. We look forward to continuing to advocate for equitable data collection practices (https://cpehn.org/about-us/blog/cpehn-introduces-bill-advancing-health-equity-with-data/) that enable all of us to access the resources and opportunities necessary to enjoy a long healthy life.
Learn More: https://cpehn.org/publications/data-exchange-framework-governance-support-letter/
Together, we can ensure we not only have a voice in the development of an improved public health and health care system but are committed leaders in the movement for racial justice and health equity.
We invite you to join us in this historic effort!

